It feels like I am about to write The Neverending story minus the magic dragons and I don’t have as cool a name as Bastian Balthazar Bux
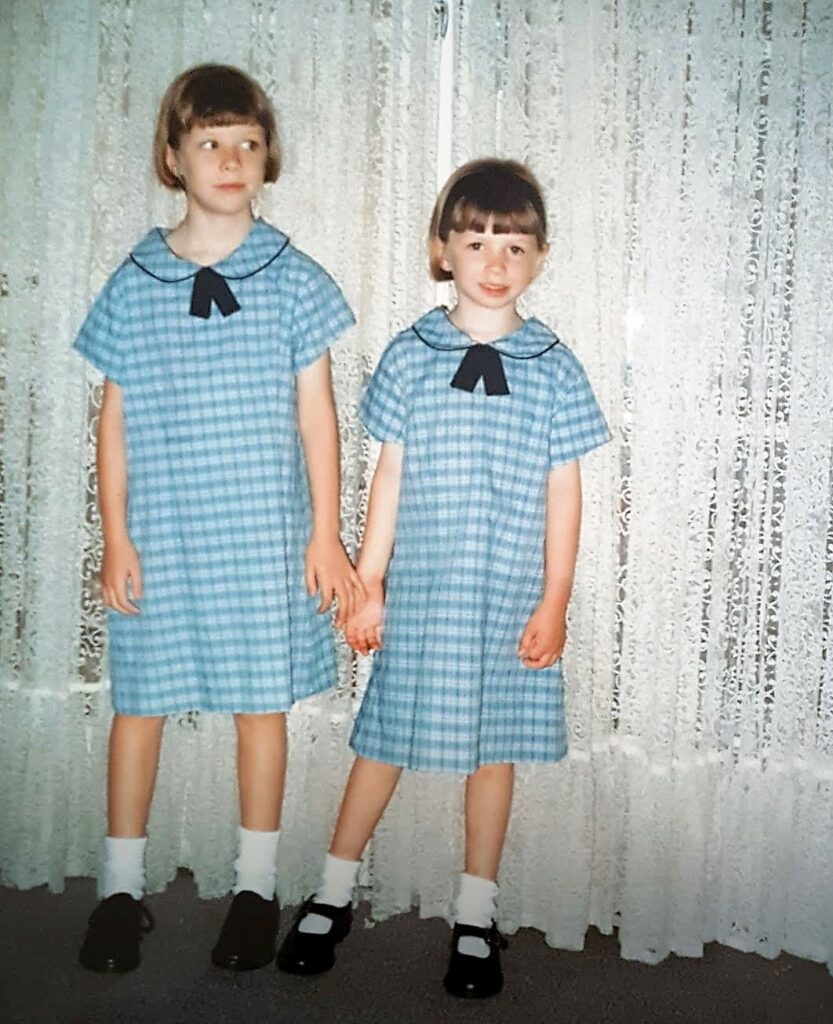
So my story with Migraine begins in 1998 as a 6 year old living in a remote and rural town experience a 6 week long persistent headache that no one knew what it was. As there was no capability of providing diagnostic testing in the town I lived in my family traveled 9 hours to take me to a hospital where I had a lumbar puncture performed.
I was discharged the same day that I had the lumbar puncture. My parents were told I had slightly raised CSF pressure and I was given a dose of steroids to take for this. I don’t remember anything about the procedure but what I do remember is leaving the hospital and then sitting in my car seat for hours in pain as we started driving home. It is crazy to me now that the hospital discharged me and didn’t specify to my parents that I should lay flat for the next couple of hours or so on but it happened. We only got four hours in to the journey home before the pain got so bad that we stopped and sought medical attention. By the time I saw the doctor at the local hospital we stopped at the pain had eased and I could bend over again so nothing needed to be done. We stayed the night in a motel and the continued the long journey home.
Apparently I initially had a good response to the steroid course for a week but the headaches returned and I was having diplopia. So two weeks later after my lumbar puncture I had a 12 hour journey to see a paediatric neurologist who admitted me for investigation. Here I was diagnosed with common migraine based on my test results and symptomology. My headaches were usually frontal and the more severe episodes were associated with nausea and photophobia. I was started on a small dose of Sandomigran for three months to see if there could be an improvement.
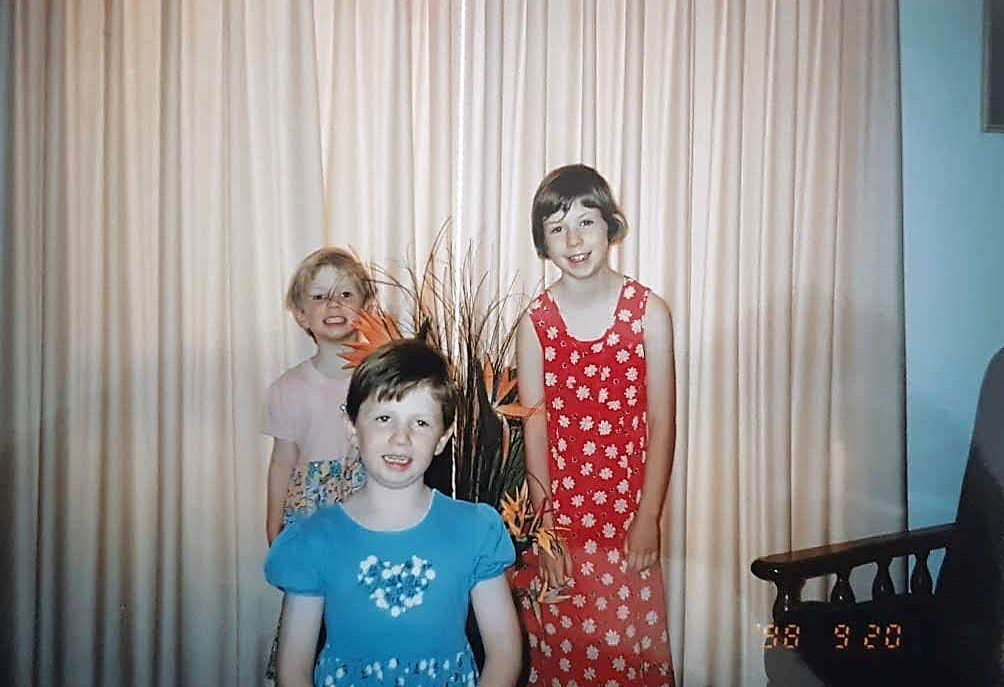
I remember my mum gave me a calendar and I marked every headache free day with a cross and after 30 free headache days we had a party. My mum called it Monica’s no more headaches party and invited school friends and neighbours. It was really sweet at the time and I didn’t know that this would be a chronic condition I battled with for the rest of my life.
So up until the last two years of high school I would have a migraine attack out of the blue over the years but it was not chronic or constant and I didn’t really think about it as it didn’t impact my life at the time.
In grade Ten I switched high schools as I had previously been bullied at my old school. This was a major stressor in my life as I had difficulty trusting people again and making friends. During this year I started experiencing more migraine attacks. I was having to have a couple of days of school a month for migraine attacks. This continued through out grade 11 and 12 as the stress of high school ramped up.

I was not on any preventive medication at this point and only took paracetamol and nurofen for my Migraine attacks. I had not seen a neurologist since 1998. I remember going to my General Practioner in 2008 crying as I was in so much pain and just didn’t know what to do. They gave me IM shot of maxalon and tramadol and sent me home with panadeine forte and maxalon to rest.
It wasn’t until 2010 when I was a 2nd year nursing student that I first was prescribed a triptan to see if it would help with acute attacks. I was also using panadeine forte or capadex to help with the pain at the time.
So in hindsight this was an exact recipe for medication overuse headaches but I had no idea. I also was not told the maximum amount of times for triptan use.

In 2012 I commenced my graduate nursing position at a large tertiary hospital. My family and I also moved from the northside or our city to the southside. I found a new GP and talked to him about my migraine attacks. He started me on my first preventive medication since I was 6. I started amitriptyline which I started at 10mg and was titrated up to 25mg. However, I was not able tolerate it as I was like a zombie due to being dizzy and drowsy as the time. I had difficulty with when to take the tablet as it makes you immediately feel tired. As a new graduate I needed to work a rotating roster including night duties and often got long runs of 10 shifts in a row as a newbie.
So I weaned off amitriptyline and was just taking panadiene forte and maxalon for my acute migraine attacks.
This all seemed to be going okay until January 2016 where I ended up in and emergency department with a 3 day long migraine that would not budge and severe photophobia. I was eventually given a largactil infusion and then discharged home. For the next 4 days my migraine attack continued and I ended up presenting to a different emergency department on day 7 of the attack with 8/10 pain. I was admitted under neurology given my persistent headache and diplopia and was given another largactil infusion and commenced on TDS indomethacin. I was given 2 bags of largactil and some intravenous fluids and anti-emetics as I was vomiting.
I was admitted under a neurologist and saw him daily. This was the first neurologist I had seen since being 6. I had an MRI brain plus MRA head and neck to rule out a dissection or stroke. I had to wait two days for the scan and those days were such a long wait of sitting in a hospital bed thinking. I was told on this presentation that I was at an increased risk of having a stroke due to having migraine disorder and being on the oral contraceptive pill. I had been on this combination pill for 7 years and not one of the general practitioners I saw during that time mentioned the increase risk of stroke and that I should not be taking this particular type of birth control.
I was discharge four days later with a clear MRI and being put back on Endep (amitriptyline) and continuing indomethacin. I was told no follow up was needed.
A month later I found myself back in the same emergency department with another severe migraine attack. I had only been pain free for a week since I was discharged from hospital in January. I was having to call sick into work for 50% of my shifts. The medical registrar called the neurologist consultant on call and uptitrated my Amitriptyline and I was to start topiramate in a week if that did not help. The doctor wrote a letter to my GP. My GP organised for me to see the neurologist which I had been admitted under in his private clinic.
Another month went by until I saw the neurologist in his private rooms. He was apologetic that I was not followed up and had to seek my own referral out. He advised me that he believed my migraines had now become chronic. He arranged an admission to a private hospital for a dexmethasone infusion and further largactil if needed. He also changed my preventative medication from amitriptyline to propanolol. I was given an acute plan to take maxalt or 900mg aspirin at first sign of an attack.
I spent two days in private hospital recieving IV dexmethasone and largactil and on discharge my pain had decreased from 8/10 to 3/10 so this was considered a success.
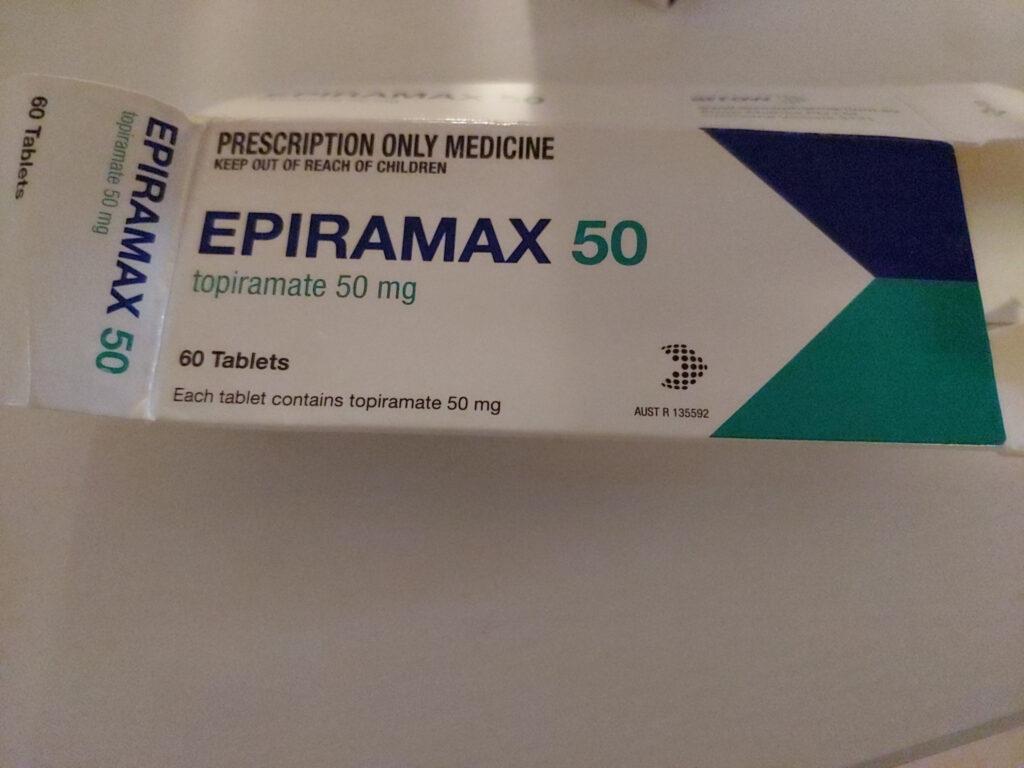
In April 2016 I was still having a daily headache since my first original attack in January and was still having frequent migraine attacks. The propanolol decreased the severity of the attacks a bit, but I was waking up every morning with a headache that was worse in the morning. Because of this my neurologist wanted to rule out raised intracranial pressure, so I had the joy of another lumbar puncture. I was also been prescribed topiramate.
During this time I came under review at work for my excessive amount of sick leave. When I requested to my manager at the time could I please drop my hours down to concentrate on my health I received the response of “you are so young what could be wrong with you”. This was not the first time nor would it be the last time that I felt the sting of the stigma of having an invisible illness.
Fast forward to May 2016 and I am on a 80mg dose of propanolol twice a day. I found myself one night feeling light-headed and having chest pain. My pulse rate was 40bpm. So back to emergency room I went, where they did some tests, monitored me for a couple hours and then just sent me home and told me to decrease my dose to 60mg twice a day.
My next follow up with my neurologist in June 2016 saw effexor 37.5mg added to my cocktail of preventors as he believed it may help due to stress being a factor. I hadn’t yet started topiramate due to the issues I was having with the propanolol and the fact that I didn’t really want to so he said hold off for now. I also received my lumbar puncture results, which were normal.
The effexor helped break the cycle and I was having more migraine free days than not. However, being on a beta blocker was making me really run down and tired. So in February 2017 I started weaning on the propranolol over the next 3 months.
All was going okay in the world of Monica’s head. I was down to one attack a month, but then in May I had 4 attacks and the headache became chronic and daily again. Not this again. I emailed my neurologist for advice and he scheduled me a sooner appointment. I was started on topiramate (and told not so subtly to actually fill the script and take it this time) and scheduled in for botox treatment in the future.
Things intially improved on topiramate and it was decided to postpone my botox treatment for a couple of months.
By the time I had my first botox in September 2017 I had just gotten back from Kenya where I had broken my leg and went back home to Melbourne for surgery. I didn’t have a neurologist in Melbourne at the time so I flew back to Brisbane on crutches to see my neurologist for botox. I looked like a right mess and my neurologist was mildly amused.

Late in 2017 I was having pins and needles in my hands and toes and started having difficulty with word finding. I would be mid-conversation and just forget words or see a word on paper and forget how to pronounce. These were all common side effects of topiramate. So when I next saw my neurologist for botox my topiramate was decreased from 50mg twice a day to just 50mg at night.
I then moved cities again in January 2018 and this time it was a more permanent move so I needed to find a new neurologist.
I found one and continued on my current regime in 2018 of botox, topiramate and effexor. I was still having days of work for migraine attacks but it was only a couple of attacks a month.
And then 2019 happened. Boy did everything go down hill. In February 2019 I had a 14 day long migraine attack which had not broken despite acute treatments I had taken. I called my neurologist and he arranged for me to admitted straight away to private hospital for a lignocaine infusion. I spent two days in a high dependency unit hooked up to monitors while I received this infusion and then another day on the ward. My pain decreased to 4/10 and I was discharged home feeling very woozy and awful.

My stay in hospital for a Lignocaine Infusion in 2019
Because I was classified as having chronic migraine and having tried at least three other preventative options I became eligible for a new medication trial in March 2019. This medication was called Aimovig. I really knew nothing about it at the time except that it was an injection that I would take once a month and was something called a CGRP inhibitor.
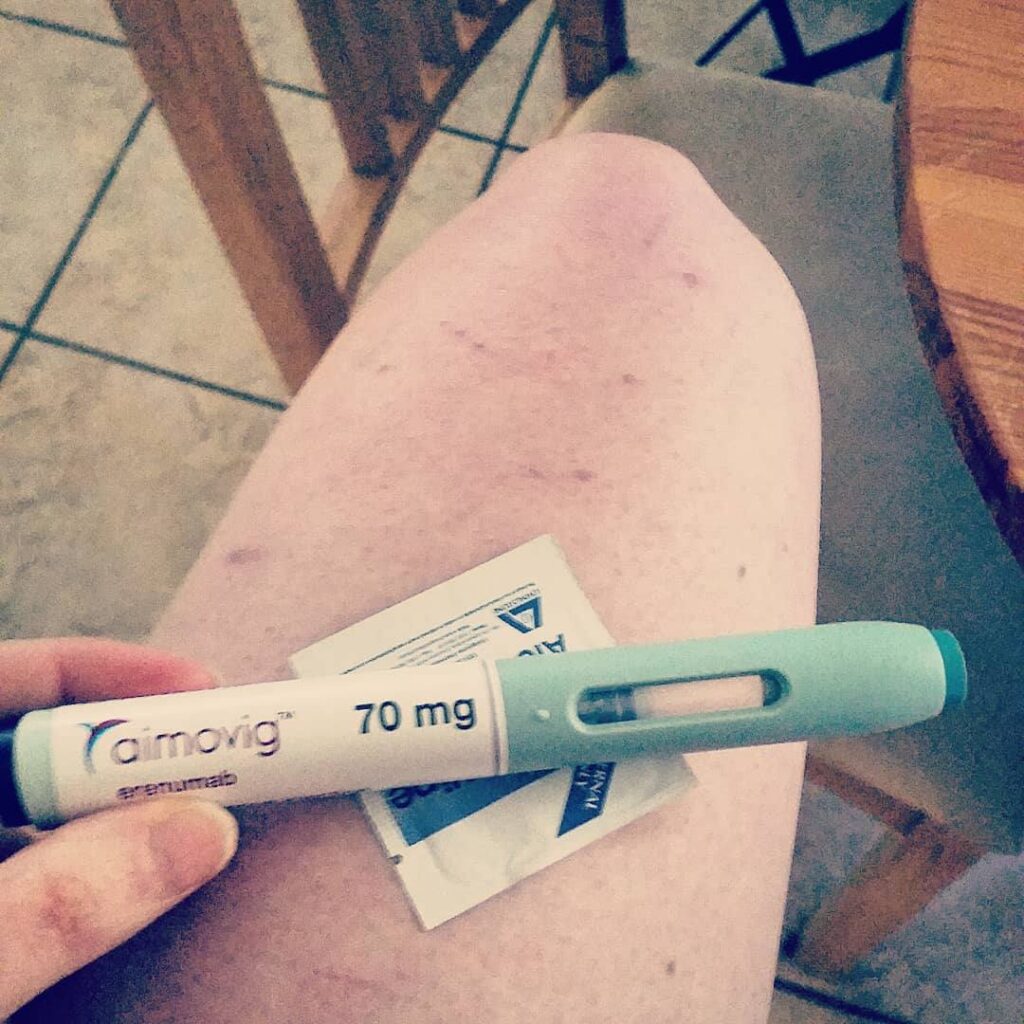
So I started on my Aimovig trial in March 2019 with low expectations but was rather surprised. It did help. It didn’t stop all my attacks but helps with intensity of them and my chronic daily headache. I was having fewer sick days from work and started being able to do a bit more.
However, my story with Aimovig was sadly short lived. I was only on a three month trial of the drug which finished the end of May 2019. To continue with the this medication it would have been $895 per month, which was a cost I could not afford. So I had to stop and just continued on with oral medications, which I was still taking.
So along came June 2019 and I went into what I would later learn is called status migraine. After 16 days of a continuous migraine attack my neurologist admitted me for a ketamine infusion. During this admission I also received bilateral occipital nerve blocks from a pain specialist to see if that could help.
Those 5 days in hospital were some of my lowest. The day before I was admitted I called my manager to tell them the plan and that I would need to be off for a week. I had already used up all my sick leave so it was all to be leave without pay. After me telling them that I needed to be admitted to hospital for treatment they told me that we would need to have a meeting about my excessive sick leave and a review to see if I was fit to continue working in the area I was. I just broke down. I felt defeated. I then went to hospital and went through a ketamine infusion and all the awful side effects of it just to have it not help at all. My neurologist told me during this admission that he didn’t know what to do next. At that time hearing that I lost all hope and did not know how I would go on. I wouldn’t be able to work and would be confined to bed.
In hindsight, I do appreciate him being honest with me as opened the conversation for us both to explore different options but at the time I felt defeated.
That migraine attack lasted 31 days and I was given a new label: refractory chronic migraine. Which basically means it is hard to treat. My topiramate was increased back up to 50mg twice a day despite previous side effects. And I was slowly weaned of effexor and swapped to duloxetine. This was to help with pain and my low mood due to the fact at the time I had a very poor quality of life.
In July I ended back in the emergency department with a migraine attack that would not stop after 3 days of acute treatment.
At this point my general practitioner wrote a medical certificate and letter to my workplace asking for at least two months off to see if things could settle. The stress of having to decide whether to call in sick or not and then the consequences of calling in sick so much were acutely weighing on me. So my treating team decided I needed time off work altogether to take a break and reassess what I am up to doing in the long run.
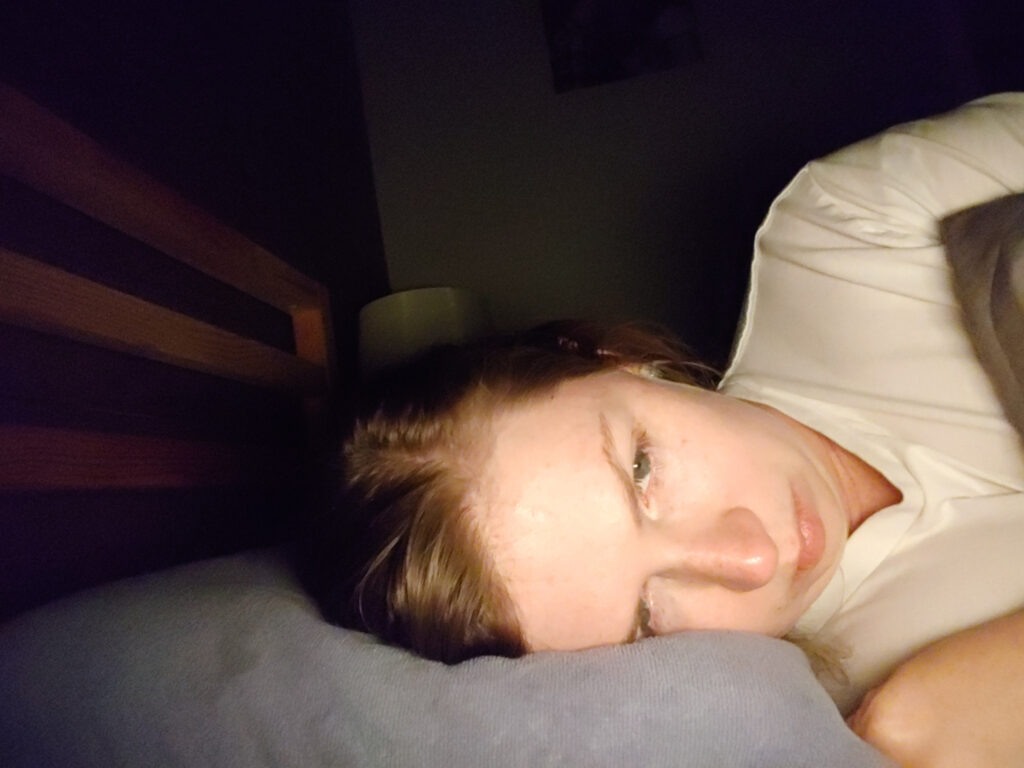
I was spending the majority of my time in bed with all the window blinds down. A good day was when I was able to take the dog for short walk otherwise he just waited until my husband got home. I didn’t eat regularly, I wasn’t able to do any house chores and it was an effort to shower myself. I felt like a burden and so guilty. My husband had not signed on to be carer and that is what he became during this time.

I was referred to the chronic pain clinic at my local hospital, which after two years in 2021 I had my first appointment.

With help of a union representative I was able to negotiate getting paid my annual leave at half pay for the time I was taking off as medical leave.
In August 2019, I traveled to Sydney to see a specific headache specialist for a second opinion. While he had the bedside manner of a dead fish he did give me suggestions for new treatment options including trialing a different CGRP inhibitor.
Come October 2019 and it was time for me to go back to work. My GP extended my medical certificate for me and wrote me a Centrelink certificate as I had run out of any type of leave. I met with one of directors for the unit I worked in and presented a letter from my neurologist outlining my condition and several accommodations that he recommended to be made. I was told these accommodations would not be able to be made and they would not help me transfer to another unit within the hospital. If I wanted to do that I would need to apply externally. The director did say though that they were happy to read my resume for me and that they were glad I was looking so much better. My biggest regret is not bringing a union representative to this meeting as I was entitled to reasonable accommodations under the law but had been point blank refused. I called the union afterwards and they said we can fight for you but it will probably be a long drawn out fight with no guaranteed outcome.
So I decided to walk away. I sent my resignation letter and my job ended in November 2019. I never even got a reply or acknowledgement of my resignation from the director I met with that day. That was when I knew I had done the right thing for me.
I then had the battle of hours of paperwork and multiple specialist appointments trying to receive access to my superannuation on medical grounds, which after months I was denied on the grounds of not being disabled enough.
I also was denied access to any Centrelink support despite having a medical certificate from my doctors due to the fact that my spouse was earning money.
I was feeling awful and had no idea what to do. I thought I would never be able to nurse again as I couldn’t get out of bed most days. I started doubting myself during this time as I had received negative comments from people and thought is it all in my head? Am I just attention seeking? I connected with an excellent therapist who specialized in treating people with chronic pain who helped me see that I was unwell and those that cared about me knew and acknowledged that.
During this Period of time there was also multiple Emergency Room visits when an Acute attack could not be controlled which were far too frequent for my liking.

My next neurology appointment in November 2019 I was signed up for a new CGRP inhibitor the Ajovy PFP trial and we talked about how if after a couple of months it was going well I could start weaning down on the topiramate. Ajovy is also a monthly injection. I was happy to finally have a plan to get this nuisance of a drug out of my life.
Later that evening after my appointment when I was trying to go to bed I suddenly a experienced sharp and extremely painful sensation in my back and groin. I could not get comfortable. I was rolling around in pain and crying. I called Healthline and spoke with a doctor. They thought it was probably muscle pain but if it is still severe to get checked by GP tomorrow to rule out kidney stones. (For the whole story check out this blog post)
Now I had previously been told topiramate could cause kidney stones but surely I couldn’t be that unlucky to get almost all the side effects.
was able to sleep for a few hours after dosing myself up with some pain killers and convinced myself that it must be muscular and I reassured my husband he should still leave for his out of state conference early tomorrow and that I likely just pulled a muscle.
The next day the pain became unbearable, and I ended up in the emergency department where I was diagnosed with kidney stones and sent home with some pain relief and antibiotics and told to try and pass the stones and keep up my fluids.
The next day I pretty much spent it on the couch. I had no appetite and by the evening I was vomiting up whatever I took in.
So back to hospital I went and this time I had an ultrasound, which showed that the kidney stone was obstructing. Then all of sudden surgery was being thrown around. I was admitted and had a urology consult.
The call to my husband that night to update him was so hard as I felt so guilty. I had already deprived him of so many opportunities due to my chronic migraine or interrupted his plans and to do it again because of a side effect of a medication for my migraine disorder was heart breaking.
He left his conference and flew back on the next available flight and arrived in the evening of the day I had surgery. I had the operation to put in a stent to allow pressure to be relieved around the obstruction. I found out this was only one of two operations I would need.

What followed this operation was two weeks of pain and discomfort as well as rebound migraine attacks being triggered by the amount of pain killers I was taking for my renal pain.
So two weeks later I had my second surgery. Thankfully they were able to successfully blast the stone and retrieve it and I was able to have the stent removed.

I just immediately felt so much better the pain and discomfort was almost gone. With feeling so much better I didn’t need to take strong pain killers but unfortunately the migraine attacks still continued from using all the pain medication.
I emailed my neurologist as soon as I got out of hospital asking for a plan to wean off topirmate as I had had enough. A couple of days later he called and I commenced the plan.
I took my first dose of Ajovy days after getting out of hospital and started slowly decreasing the topiramate until I was finally free of the drug being in my system.
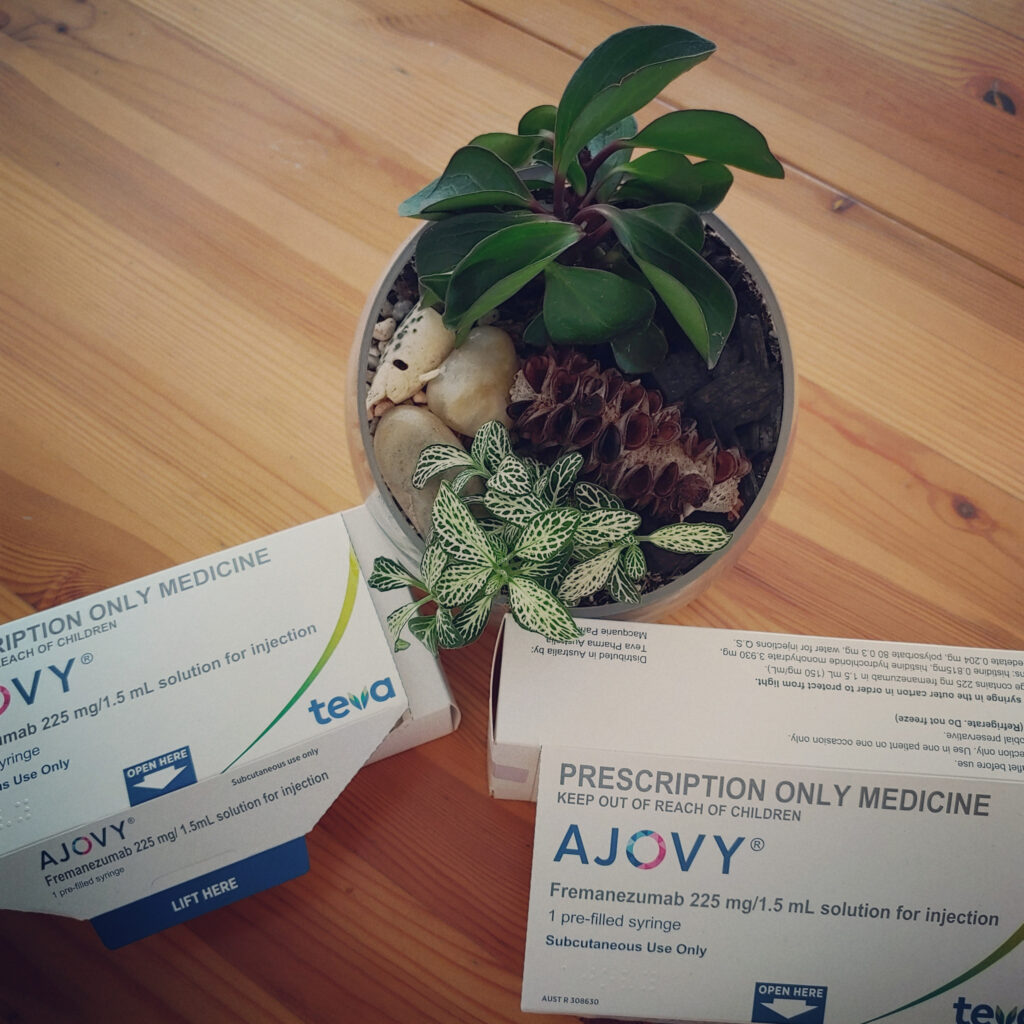
This was the worst 6 months I had experienced which resulted in multiple emergency department visits and hospitalisations. Out of 183 days prior to starting Ajovy, I had a severe attack on 126 of them. My quality of life was poor at best. I felt bed bound and when I did try and go out I often struggled and felt worse afterwards.
Since starting Ajovy in December 2019 I have only been to hospital twice for booked Ketamine infusions and a handful of times to Emergency department for an acute attack. In the year of 2019 I had 186 attack days out of 365 days. In 2020 my Migraine attack days had more than halved and decreased to 91 out of 366 days. More importantly than that, I feel like I have a life again. I don’t have a chronic daily headache everyday anymore. The severity and length of my acute attacks has decreased. I have energy and am able to get up out of bed and do things. I have even been able to work part time as well as do extra shifts helping as an immuniser.
Ajovy was recommended in the March 2020 meeting of the PBAC to be listed on the PBS, but as yet the medication has not been listed. It has been recommended to be put on the PBS but under the same cap as botox. While this is great news that it was approved it is not likely to be put on the PBS until the cap is raised as this class of drugs is expensive to manufacture. So I remain unsure how long I will have access to this life-changing drug on the trial and what the cost will be once it concludes.
So this is where I am at the moment. I have finally found a successful treatment but am not sure for how long I will be able to use it for.

What I have taken away from reflecting and writing down my whole story is the importance of advocating for yourself and find a good general practitioner you can trust. It is so important to have a migraine action plan created for you early on rather than relying on opioids. It is also important to do your own research as well, so that you can be an informed participant in your health care decisions. But most of all don’t let people make you feel like you aren’t allowed to be unwell or as sick as your are. Migraine is a neurological disease and should be treated accordingly with respect and empathy.
Thank you for reading my story and I would love for you to share yours with me sometime.
Monica x

